The challenge
It might surprise you that high blood pressure (hypertension) is one of the most common causes of death in the world. High blood pressure leads to heart disease and strokes, and it kills more people than all infectious diseases combined. In many countries, like the US or India, about 1-in-4 adults has high BP, which translates into hundreds of millions of people who are at risk.
The good news is that most deaths from high BP are avoidable. There are several things that countries must do to get a handle on the problem. One of them is to measure where treatment for hypertension is working and where it could be improved. The tech team that builds Simple is responsible for helping clinicians and health officials measure outcomes so patients lower their BP to a safer level, health facilities improve BP control rates, states improve control at the population level, and that as a result heart disease, strokes, and deaths are avoided.
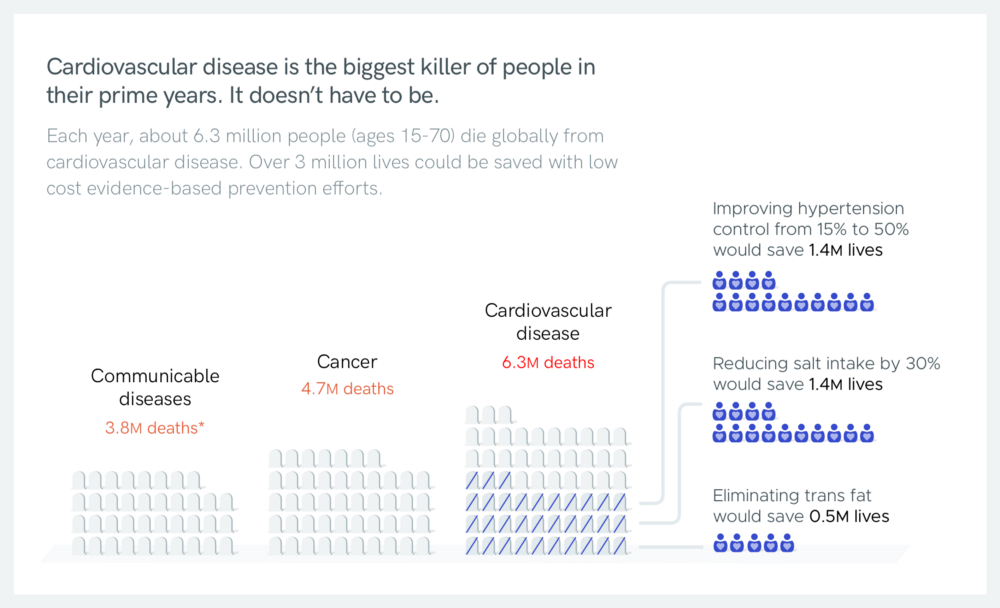
By using evidence-based methods, it’s possible to save 3 million lives every year from cardiovascular disease
Measuring outcomes is really difficult in places where doctors and nurses are already overworked. In countries like India and Bangladesh, a doctor or nurse frequently sees more than 100 patients in a single day. A typical clinic visit in the US is about 15 minutes but in India an average encounter is less than 5 minutes. In the US, clinicians feel burdened by data entry tasks — given the choice, they would maximize their time talking directly to patients, without their eyes glued to a computer screen. So, it’s unsurprising that busy clinicians in India are even less inclined to record data about patients.
When we ask health care workers in India what they would like to see in new software, they consistently tell us: “Just please don’t make my work harder.”
In many places with high volume patient care there is minimal longitudinal data about patients. Each patient who comes into the facility is treated like a new patient, even if they’ve been there a hundred times before. That makes it difficult to improve the clinical outcomes for patients and improve the quality of the overall system. If you don’t know what a patient’s previous BP was, how do you know if they’re improving? If you don’t know the percentage trend of patients with controlled BP, how do you know if your system is improving?
With Simple, we’re taking a radically simple approach to help clinicians to manage their patients with high blood pressure. Our goal is to help doctors and nurses to record a patient’s high BP treatment encounter in less than 15 seconds. Today, after 11 months of use in a handful of pilot districts in India, we just crossed the milestone of 125,000 patients managed in Simple.
What have we done so far to get there?
Ask for the bare minimum
Many medical record systems are designed by administrators or by public health officials. They’re often disconnected from the day-to-day work of busy healthcare workers, so it seems like no big deal to add ‘interesting’ or ‘useful’ data entry fields. As we’ve seen with complex systems, if you ask for too much data, either clinicians don’t use the software at all or they enter low quality data: “garbage-in garbage-out.”
We aim to only ask for the bare minimum to 1) improve an individual’s care and 2) create feedback loops to improve BP control rates across a health system. Every time we consider adding a field, we ask tough questions: is it really necessary? Right now, we only ask clinicians to enter basic patient identification, 4 short medical history questions, today’s BP, and the patient’s current BP medications. That’s it.
By focusing on only what matters most, we can significantly reduce how much time clinicians spend entering data into Simple.

*In June we introduced a patient ID we call a “BP Passport” with a scannable QR code.
Easy to learn, easy to deploy
Usually, adopting new clinical software is a pain. Training staff and changing workflows takes up significant staff time. Easy-to-use software is easier for healthcare workers to learn and easier for managers to adopt. We aim for a nurse or doctor to be able to install Simple from the Play store, watch a 5 minute Youtube tutorial , practice for 30 minutes, and then start recording patient visits. We’re not quite there yet (trainers still conduct short sessions with staff and give out handbooks) but Simple is relatively fast to learn and many trainings are done at the point of care.

Partly because Simple is a fairly low burden for health workers, in only 9 months it has been deployed to 363 government health care facilities in India. Of those facilities, 342 (94%) are active*, which is a strong adoption rate for new software.
“94% active adoption is extremely impressive for health information technology in global health.” — Dr. Gregory Schmidt, Indiana University Center for Global Health and AMPATH Kenya
Using personal Android devices
Many health systems acquire thousands of tablets or computers for their staff. It’s a huge investment and a high hurdle for deployments. We took an unusual approach: ask healthcare workers to use their personal Android smartphones, where they’re willing to do so.
You might think that using personal devices is primarily a cost-saving tactic, but buying $100 devices for 400 clinics isn’t that pricey. Personal devices have a few surprising advantages:
- The best device is the one that’s with you when you’re seeing a patient: If a nurse can pull a device from her pocket and record a patient she doesn’t have to hunt down the equipment.
- Internet access is more reliable: If a facility has unreliable network coverage, the nurse can work offline all day (see below). When she goes home and passes through a reliable mobile network area, Simple will sync the patient data to secure cloud storage overseen by the government.
- Devices are maintained: When a screen cracks, the nurse fixes it. When Android software needs to be updated, the nurse updates it. Hardware purchased by clinics often end up sitting on the shelf collecting dust, while a clinician’s personal device is cared for.
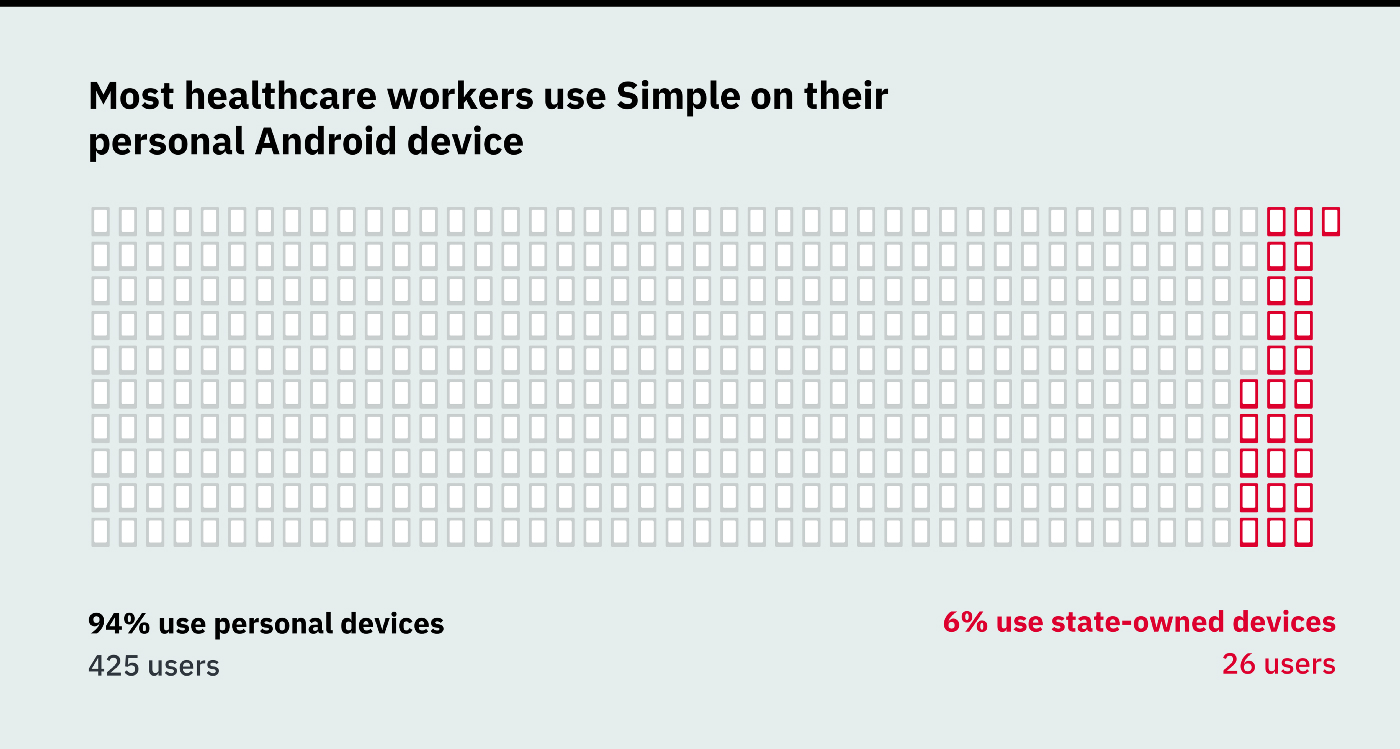
Personal device usage data as of Aug 31, 2019
Using personal devices might not have been possible in a place like India 10 years ago. But lowered data costs and reduced hardware prices have significantly improved access in recent years. We still help purchase well-priced Android hardware where necessary but use of personal devices has gone much better than we anticipated.
The benefits of personal devices mean that Simple can be deployed quickly and widely with less logistical complexity.
Go offline-first
At the outset of the project, the Android engineering lead was emphatic that the software had to be designed offline-first. That means that the app has to be fully functional with no internet connection for days at a time. Sounds basic, but going offline-first introduces complexity and duplication between the back-end and front-end systems. Despite the added effort this decision was 100% worth it.
It may seem a bit obvious to go offline-first in places where there is really low connectivity. But, connectivity is actually pretty good even in rural India where we deployed. The biggest benefit of going offline-first is that the app is really snappy no matter if you’re in 1 bar of mobile service or on a wifi connection. When a clinician is in front of a patient, they need to get their work done, not wait for the app to send messages to-and-from the cloud. Every screen in Simple is snappier because it was built offline-first.
Before we started, we saw other systems, like eHealth Kerala’s tablet-based EMR for frontline health workers, going offline-first and it’s a smart choice — this is a good trend we see in lightweight EMRs.
Work with frontline health workers
We are lucky to get to work with nurses, doctors, pharmacists, and Cardiovascular Health Officers. We get to work with many clinicians by observing their care in the field, asking questions, and trying new features with them. We work with people in a variety of ways:
- Observe real clinical care
- Ask questions
- Prototype and test new ideas with health workers in the field
- Come up with solutions together

Members of the Simple user experience team (Dhruv, Tanushree, and Akshay) working with clinicians
In the last 16 months, we have conducted dozens of user tests and observations. We disseminate the knowledge from our user testing and customer support team to our engineers and product team to help make better empathetic software decisions.
We also take our customer support seriously. We hired a deployment coordinator, Praveen Kumar, and he is in daily contact with nurses, doctors, and surveillance officers and relays their input to the development team. In addition, each month he draws up a high-level and hyper-useful report (see an example) that summarizes the problems that our users face.
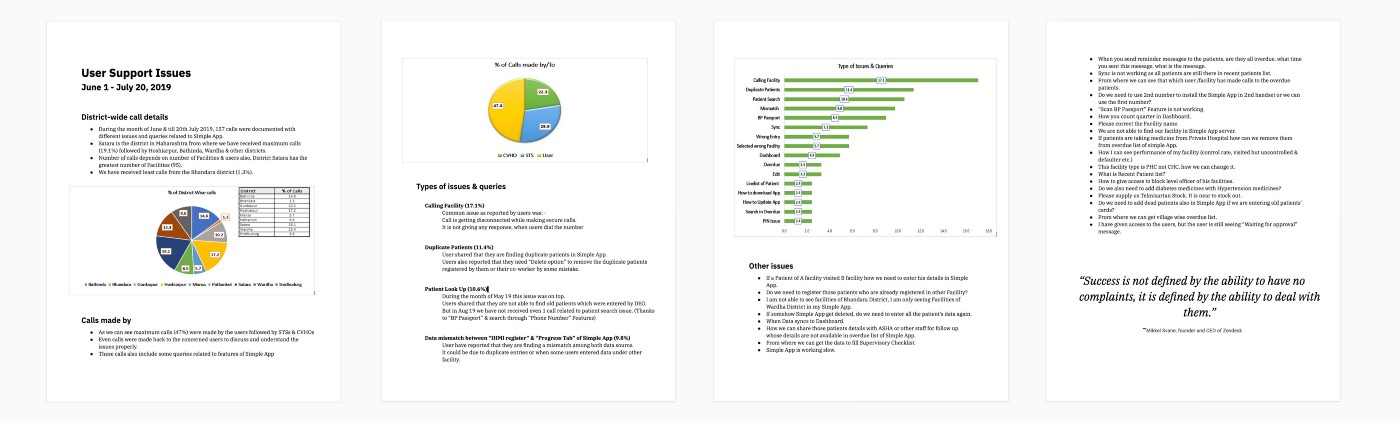
An example of an actual customer support report prepared in India. See the Google Doc
Made in India
85% of our paid tech team is Indian. Together, we’re creating software for India and then the world. Sometimes we see teams that write a software specification and hand the labor of development to a team of engineers — it’s not a good way to make great software. India is home to some of the strongest tech talent in the world and our tech team is an integrated 3-legged stool of design, engineering, and product.
A truly agile approach
Let’s be honest, we don’t have all the answers. We often head in the wrong direction and make software that clinicians don’t like. So, we don’t try to design perfect software. Instead, we build in bursts and we put our prototypes and software in our users’ hands as quickly as possible so we can learn what works and what doesn’t work in the field (obviously, without compromising safety and security). Usually we test prototypes within a few weeks, before we even start development.
We’re taking a lowercase ‘a’ agile approach. We generally adhere to normal Agile™ development models but we’re not bound to them. Our emphasis is on learning early and often, measuring and iterating. This has sometimes meant that we already had to refactor code, but the nimbleness of not trying to do it “perfectly right” the first time is worth it.
We were also ruthless in pursuing a minimum viable product (MVP) for launch, which allowed us to get the first functioning version of Simple into users’ hands only 6 months after kicking off development. Many key features were missing from the first version of the app. For example: patient search was clunky, it wasn’t possible to contact overdue patients, and there was no feedback to nurses to track their progress. Remember the original iPhone? iPhone version 1.0 launched without an App Store and had only 16 basic apps. Similarly, we launched light, which allowed us to learn from our users and our roadmap is dictated largely from their needs.
The excellent draft of India’s National Digital Health Blueprint wisely suggests to start with a simple foundation and build from there.
Build on the experience of others
Simple is a pretty basic app. It’s not like we’re on the bleeding edge here. A lot of our approach is building on the experience of people like Dr Prabhdeep Kaur, Dr Ashish Krishna, Dr Tom Frieden, Dr Marc Jaffe, and Dr Terry Cullen — people who have put in decades of work and learned many lessons from working on many public health projects.
We’re often adapting the analog approach that has worked in other places and adapting it to scale in the digital world. We are trying to leverage the parts of the paper records systems that worked phenomenally and adapt them to the possibilities of a digital world.
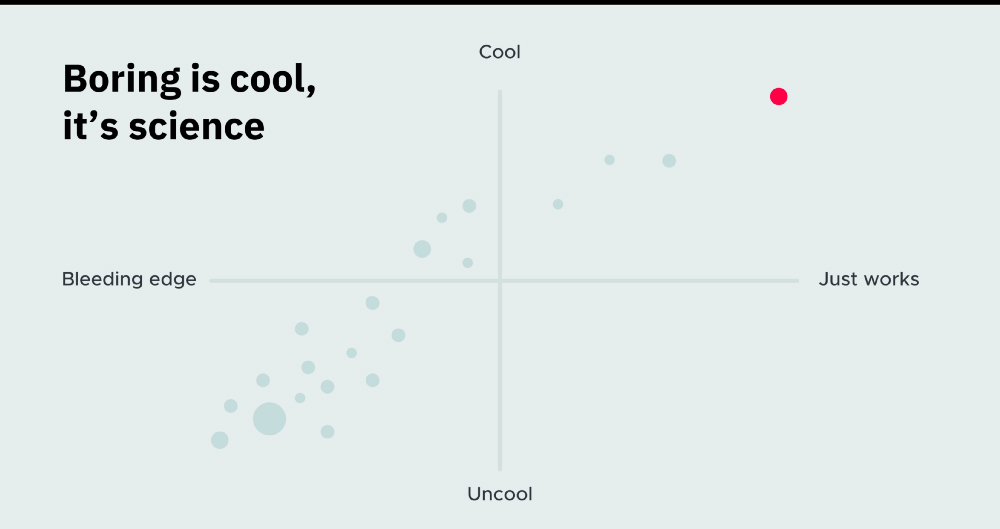
This one chart is just made up… :)
Avoid the buzz
AI, machine learning, and blockchain are all cool. But, it is a bit astonishing how often they come up in health tech discussions where ‘boring’ software will get the job done. What gets us excited is basic, well-built platforms, applied at scale to save lives.
It's not about the software
This might sound weird, but our goal isn’t to make Simple successful. The goal is to save lives from heart attacks and strokes by strengthening health systems and helping them increase their patients’ blood pressure control. Software isn’t the solution… it is one part of a puzzle that our colleagues and partners tackle with us. There is a risk that “tech” is a bolt-on solution as opposed to an integrated piece of a broad program. If we are to succeed in saving lives, it will be because people are empowered to do their hard work and have the right feedback to treat patients to the best of their ability.
What's next?
We haven’t written much about Simple until now because we didn’t have any evidence that any of our approaches were good ones. It’s still a bit premature to claim any successes — one hundred thousand patients is a good start, but hypertension affects hundreds of millions of people.
In the next year, Simple will be deployed in many more clinics in India and will deploy in other countries in the next 6 months. We will also be adding diabetes support (of course in the “simple” way) at the request of the India Hypertension Control Initiative.
As we go, we will try to share our successes and mistakes more frequently.

Patients with “BP Passports”, an ID system for Simple. Over 50,000 BP Passports have been distributed to patients.
Thanks to Dr Terry Cullen, Dr Gregory Schmidt, Dr Tom Frieden, Farzad Mostashari, Dr Andrew Moran, Dr Prabhdeep Kaur, Tanushree Jindal, Akshay Verma, Tim Cheadle, Erin Sykes, and everyone else who contributed to the writing and editing of this article. Also, thank you to everyone who is part of the India Hypertension Control Initiative who make Simple successful through their hard work every day.
Footnotes
* Active facilities: 342 facilities recorded > 15 patients in the last 30 days, 323 facilities recorded > 20 patients in the last 30 days, 156 facilities recorded > 100 patients in the last 30 days